31/08/2023
The liver, a powerhouse organ, is a cornerstone of overall wellness. It plays a pivotal role in the body’s metabolic processes, detoxification, and digestion. Despite its resilience, the liver is susceptible to damage from various factors, including excessive alcohol, toxins, and viruses as well as diet and lifestyle. Liver diseases can be silent for years, often detected only when they have progressed to a severe stage. This makes regular liver health checks crucial for the early detection and management of potential liver conditions. Randox Health recognizes the importance of liver health and includes a comprehensive liver function test in its health packages. This article will delve into the significance of liver health, common liver diseases, and the role of Randox Health in providing personalized health insights.
The Importance of Liver Health
The liver, the body’s largest internal organ, performs over 500 vital functions1. It processes virtually everything we eat, drink, breathe, or absorb through the skin. It metabolizes nutrients from food to produce energy, breaks down alcohol and drugs, and removes harmful toxins from the body. The liver also produces bile, a substance needed to digest fats and absorb vitamins A, D, E, and K. Moreover, it plays a crucial role in regulating blood sugar levels, cholesterol levels, and protein synthesis.
Despite its critical functions and its ability to regenerate, the liver is not invincible. Prolonged exposure to harmful substances, such as excessive alcohol, toxins, or certain medications, can damage the liver, leading to liver diseases. Low physical activity and an unbalanced diet are also known to have a significant impact on the progression of liver diseases. Physical inactivity and dietary overconsumption can lead to high levels of lipid accumulation in the liver, playing a part in the progression of liver diseases. These diseases can range from non-alcoholic fatty liver disease, and cirrhosis, to liver cancer.

Randox Health and Liver Health
Randox Health’s comprehensive health packages include extensive liver function tests. These tests measure various biomarkers, providing a detailed picture of liver health. They can detect early signs of liver disease, even before symptoms appear, enabling timely intervention.
Liver function tests measure levels of various enzymes and proteins in your blood that are produced by liver cells. If the liver is damaged or diseased, these substances can leak out of the liver cells and show up in the blood.
For instance, the tests measure levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), albumin, and bilirubin. Elevated levels of ALT, AST, and ALP can indicate liver damage, while low levels of albumin and high levels of bilirubin can suggest liver disease.
Randox Health’s liver function tests also include a test for gamma-glutamyl transferase (GGT). This test is particularly sensitive for detecting bile duct problems. Elevated GGT levels can indicate bile duct disease or liver disease.
By providing a comprehensive analysis of these biomarkers, Randox Health’s liver function tests offer a proactive approach to liver health. They enable individuals to understand their liver health status and take necessary actions if abnormalities are detected.
Common Liver Diseases
Liver diseases are a global health concern. They include conditions such as:
Non-Alcoholic Fatty Liver Disease
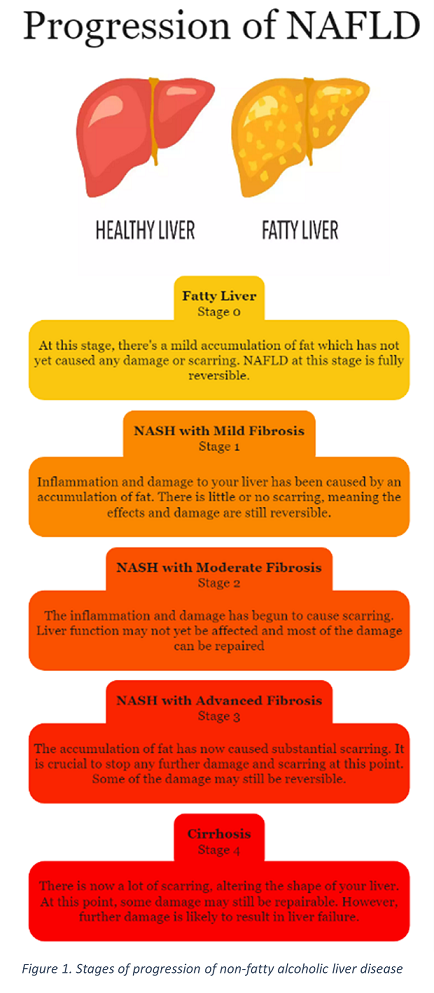
Non-alcoholic fatty liver disease (NAFLD) is a collection of diseases defined by the accumulation of fat in the liver when no other causes for this hepatic steatosis are apparent (e.g. in the absence of excessive alcohol consumption).
Fatty liver disease can range in severity from relatively mild non-alcoholic fatty liver (NAFL) to severe and life-threatening liver damage, such as non-alcoholic steatohepatitis (NASH) and cirrhosis (scarring of the liver).
Estimated to affect 1 in 5 people in the UK, rates of NAFLD are rising with levels of obesity2. Many cases of NAFLD are weight-related, however, it is possible to develop NAFLD at a healthy weight. Factors that can increase your risk of NAFLD are obesity, type 2 diabetes, a diet high in unhealthy food or drinks, low levels of physical activity, high cholesterol, high blood pressure and other conditions associated with insulin resistance, such as polycystic ovary syndrome2.
NAFLD is often asymptomatic, even at its later stages. Commonly, people with NAFLD complain of tiredness, fatigue or lethargy and discomfort on the upper right side of their stomach, where the liver is found. Other symptoms may indicate more severe liver disease. If you develop any of the following and are in one of the high-risk groups discussed above, you should seek medical attention: jaundice (yellowness of the skin and eyes), easily bruising, dark urine, swelling of the stomach area, vomiting blood, dark tarry faeces, encephalopathy (periods of confusion, mood changes or poor judgement), itchy skin2.
Cirrhosis
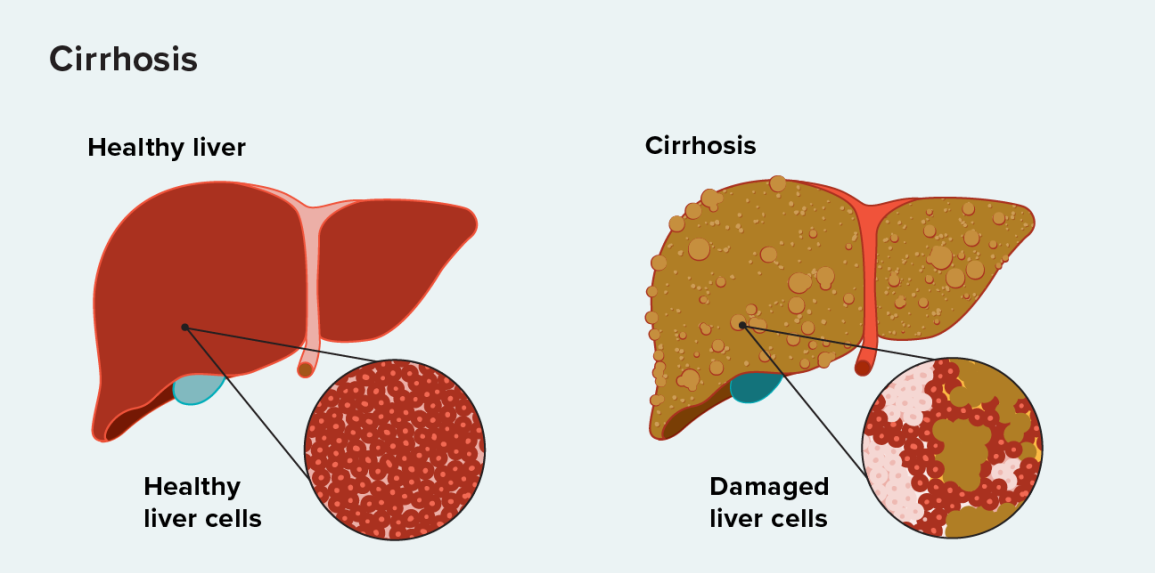
Cirrhosis gets its name from the Greek word meaning ‘yellowish’ due to the change in skin colour associated with severe cirrhosis.
It is defined as fibrosis or scarring of the liver as a result of chronic liver damage3. This fibrosis inhibits the proper function of the liver. Cirrhosis is often referred to as end-stage liver disease as it is commonly the result of the other conditions discussed in this article. Common symptoms include fatigue, nausea, unexplained weight loss and red patches appearing on the hands and body3. Severe cirrhosis can be identified by the yellowing of the skin and eyes, blood in the vomit, itchy skin, easy bruising or bleeding and loss of libido.
There is currently no cure for cirrhosis however, management of cirrhosis can include changes in lifestyle such as eliminating alcohol intake, losing weight, and treating the underlying issue that causes cirrhosis. In severe cases, transplantation may be the only option3.
Cholestasis
Cholestasis is a condition where bile cannot flow from the liver to the duodenum. The bile gets backed up in the liver, causing damage to the liver cells. Cholestasis can be caused by various diseases, including gallstones, certain medications, and liver diseases. Symptoms may include jaundice, dark urine, pale stools, and itching8.
Other Complications
NAFLD can play a role in the progression of other diseases and complications. Increased levels of fat in the liver have been shown to be associated with an increased risk of developing diabetes4 and cardiovascular diseases, such as stroke and heart attack, which are the largest cause of mortality among NAFLD patients5. Other conditions associated with NAFLD include chronic kidney disease, obstructive sleep apnoea syndrome, polycystic ovarian syndrome, and extrahepatic malignancies, such as colorectal cancer5.

Alcoholic Liver Disease
Like NAFLD, Alcoholic Liver Disease (ALD) is a wide spectrum of conditions including steatosis, acute alcoholic hepatitis with or without cirrhosis and hepatocellular carcinoma (HCC). ALD can also occur as a comorbidity with NAFLD or hepatitis C (HCV) viral infection, worsening the prognosis3.
ALD develops from both heavy alcohol intake and frequent alcohol abuse, most of those diagnosed report heavy alcohol consumption over years or decades3. Other important risk factors include female sex, obesity or excessive weight, and HCV infection. There is a risk of ALD becoming HCC which is discussed in more detail in the next section. Diagnosis of ALD involves measuring the AST/ALT ratio and body mass index (BMI)3.
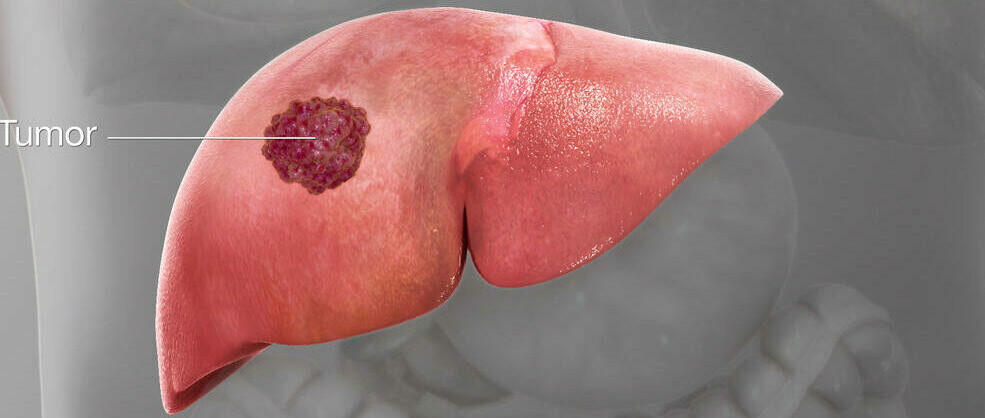
Liver Cancer
Liver cancer is a serious condition with a high mortality rate. It often develops in the context of chronic liver disease, particularly cirrhosis7. The two most common types of liver cancer are HCC and intrahepatic cholangiocarcinoma (ICC). HCC is the most common liver malignancy in the world and its prevalence is increasing8. It is a common clinical manifestation associated with chronic liver diseases such as those discussed in this article.
ICC is a form of cancer that originates from the lining cells of the bile ducts located both within and outside the liver, specifically near the segmental biliary ducts. While it’s often associated with risk factors such as chronic hepatitis, cirrhosis and inflammation of the bile ducts, most cases don’t have a clearly identified risk factor9. Risk factors for all forms of liver cancer include chronic infection with hepatitis B or C, cirrhosis, certain inherited liver diseases, diabetes, obesity, and excessive alcohol consumption7.
Intervention
A well-balanced diet is the first step to improving your liver health. Adopting a diet high in fruits, vegetables, whole grains, lean proteins, and healthy fats, like olive oil, can reduce the rate at which fats accumulate in your liver.
However, rapid weight loss or ‘crash diets’ can be detrimental to your liver, so gradual and sustainable weight loss is crucial. If you have any concerns about your current diet, you should consult your physician or nutritionist. A regular exercise routine goes hand-in-hand with a healthy, balanced diet and is just as critical for managing NAFLD and maintaining liver health.
A combination of aerobic and resistance exercises is the best approach; combining exercises such as running, cycling, or swimming with weightlifting or bodyweight exercises has been shown to be effective in treating NAFLD10.
Just like diet, dramatic changes can have negative effects so it’s important to begin with achievable goals which you can sustain.
Where can I get Liver Testing?
Randox Health’s comprehensive health packages, which include an extensive liver function test, providing a proactive approach to liver health. By detecting potential liver conditions early, they enable timely intervention and management. In a world where liver diseases are a significant concern, Randox Health offers a beacon of hope. By providing personalized, comprehensive, and timely health insights, it empowers individuals to take charge of their health, ensuring a safer and healthier life.
References:
- John Hopkins Medicine. Liver Health. www.hopkinsmedicine.org. Published 2023. https://www.hopkinsmedicine.org/health/conditions-and-diseases/liver-health
- Pouwels S, Sakran N, Graham Y, et al. Non-alcoholic fatty liver disease (NAFLD): a review of pathophysiology, clinical management and effects of weight loss. BMC Endocrine Disorders. 2022;22(1). doi:https://doi.org/10.1186/s12902-022-00980-1
- Dunn W, Shah VH. Pathogenesis of Alcoholic Liver Disease. Clinics in Liver Disease. 2016;20(3):445-456. doi:https://doi.org/10.1016/j.cld.2016.02.004
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: a Cancer Journal for Clinicians. 2018;68(6):394-424
- Clark T, Maximin S, Meier J, Pokharel S, Bhargava P. Hepatocellular Carcinoma: Review of Epidemiology, Screening, Imaging Diagnosis, Response Assessment, and Treatment. Current Problems in Diagnostic Radiology. 2015;44(6):479-486. doi:https://doi.org/10.1067/j.cpradiol.2015.04.004
- El-Diwany R, Pawlik TM, Ejaz A. Intrahepatic Cholangiocarcinoma. Surgical Oncology Clinics of North America. 2019;28(4):587-599. doi:https://doi.org/10.1016/j.soc.2019.06.002
- Overview – Cirrhosis. NHS. Published 2019. https://www.nhs.uk/conditions/Cirrhosis/
- Padda MS, Sanchez M, Akhtar AJ, Boyer JL. Drug-induced cholestasis. Hepatology. 2011;53(4):1377-1387. doi:https://doi.org/10.1002/hep.24229
- Angelini C. The role of corticosteroids in muscular dystrophy: A critical appraisal. Muscle & Nerve. 2007;36(4):424-435. doi:https://doi.org/10.1002/mus.20812
- Ala A, Walker AP, Ashkan K, Dooley JS, Schilsky ML. Wilson’s disease. The Lancet. 2007;369(9559):397-408. doi:https://doi.org/10.1016/S0140-6736(07)60196-2
- Pietrangelo A. Hereditary Hemochromatosis: Pathogenesis, Diagnosis, and Treatment. Gastroenterology. 2010;139(2):393-408.e2. doi:https://doi.org/10.1053/j.gastro.2010.06.013