29/09/2023
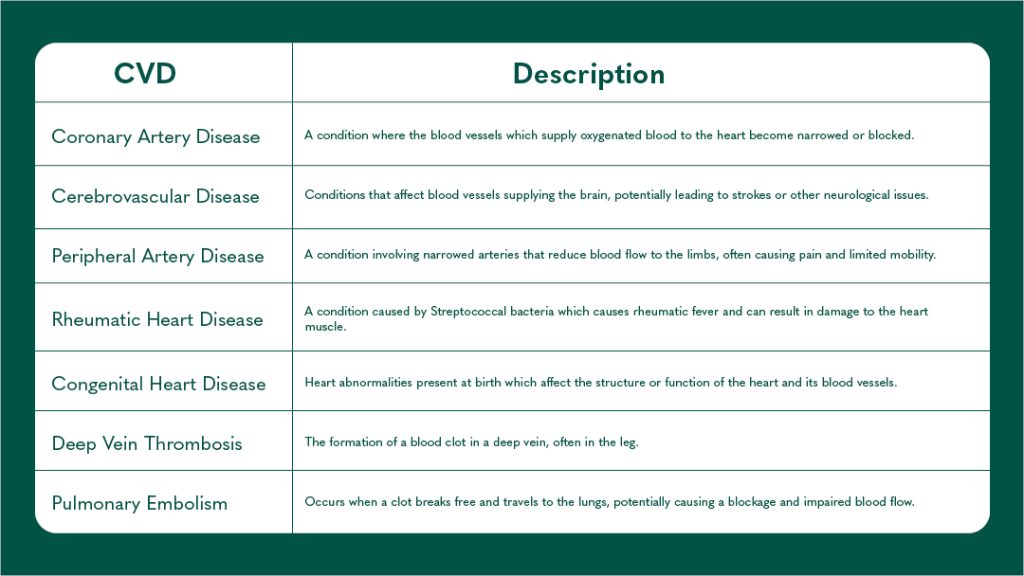
On average, your heart will beat over 3 billion times over your lifetime1, pumping blood around the 60,000 miles of blood vessels in your body2. You probably didn’t need these statistics to realise how important your heart health is, yet many of us don’t take appropriate action to maintain or improve our cardiovascular health. Cardiovascular diseases (CVDs) refer to a collection of diseases which affect the heart and blood vessels. They are the leading cause of death globally, accounting for 17.9 million deaths in 2019, a staggering 32% of all deaths that year3. There are various types of CVD, some of which are detailed in the table below. However, 85% of deaths from CVDs are attributed to heart attack or stroke3. These acute events are most often caused by the blockage of a blood vessel which restricts or inhibits blood flow to the heart or brain.
Table 1. Cardiovascular diseases and definitions
Heart Disease and Failure
Heart Disease is a term that encompasses a range of CVDs that affect the heart’s structure and function. Examples include coronary artery disease (CAD), heart failure, arrhythmias, congenital heart defects and more. Many types of CVD, including most types of heart disease, are the result of a buildup of plaque on the inner wall of the arteries. These plaques are made of fats, cholesterols, calcium, and various other cellular components. Given sufficient time, these plaques grow and harden and cause the arteries to narrow and stiffen, resulting in reduced blood flow4. The process of plaque development is known as atherosclerosis. Atherosclerosis in the coronary artery (that which supplies oxygenated blood to the heart) is known as CAD5, but plaque formation can happen in arteries and veins throughout the body, causing conditions such as peripheral artery disease and cerebrovascular diseases3.
As is the case with many CVDs, heart disease can progress without the onset of symptoms6. Commonly, the first sign of heart disease is a heart attack. A heart attack, otherwise known as myocardial infarction, describes the sudden and severe reduction of the heart’s blood supply due to atherosclerosis or a blood clot6.

Cholesterol (total, LDL, and HDL), triglycerides, and apolipoproteins (ApoA1 and ApoB) play important roles in heart disease. Elevated levels of total cholesterol and LDL cholesterol are associated with an increased risk of atherosclerosis and heart disease, while higher levels of HDL cholesterol are beneficial for heart health7. Triglycerides, when elevated, may also contribute to the risk of heart disease8. Apolipoproteins, such as ApoA1 and ApoB, are proteins that bind to lipids and can provide additional information for predicting cardiovascular risk9. Lp(a), or lipoprotein(a), is a type of lipoprotein in the blood that has been linked to an increased risk of heart disease and atherosclerosis due to its role in promoting plaque buildup in the arteries10. Monitoring and managing these lipid markers are crucial for assessing cardiovascular risk and guiding treatment decisions.
Early detection of heart disease can improve outcomes dramatically. If detected at the pre-symptomatic phase, various, inexpensive therapeutic strategies can significantly reduce the risk of developing heart disease, for example, those who display high blood pressure can see benefits by reducing their salt intake.
Some things which affect your risk of heart disease can’t be helped such as age, sex, and family history of heart disease11. However, there are many modifiable risk factors which increase your risk of developing heart disease. These include unhealthy diet, physical inactivity, smoking, high blood pressure, high cholesterol, diabetes, overweight or obesity, and stress11. By identifying your risk early, you can take proactive steps to improve your overall health and your risk of developing heart disease.
Read more about blood pressure and how to ‘know your numbers’ in our blog here.
Stroke and Atrial Fibrillation
There are two main types of strokes: ischemic and haemorrhagic. Ischemic strokes are those caused by a blockage in the blood vessel that supplies the brain, while haemorrhagic strokes are caused by bleeding in or around the brain, the result of a burst blood vessel12. Ischemic strokes are commonly caused by atherosclerosis13 but may also result from a blood clot that forms in a blood vessel in the brain (thrombosis) or a clot that originates in the heart and travels through the vasculature to the brain (cardioembolism)12.

The data shows that high blood pressure, smoking, heavy alcohol consumption, and obesity. Studies also show that elevated levels of total cholesterol, LDL cholesterol, and triglycerides are associated with an increased risk of ischemic stroke. Conversely, low levels of total cholesterol are associated with an increased risk of haemorrhagic stroke14.
Under normal conditions, the heart contracts and relaxes at a steady pace. In those who suffer from atrial fibrillation (AF) the upper chambers of the heart, known as the atria, fall out of step, beating irregularly or quivering. This affects the heart’s function and can cause pools of blood to form, increasing the risk of blood clots. For this reason, those with AF are at a 5x increased risk of developing a stroke and are at double the risk of heart-related death15.
Diabetes Health
The relationship between CVDs and diabetes is intricate and closely intertwined. Diabetes, especially type 2 diabetes, significantly increases the risk of developing cardiovascular complications16. Diabetes can damage blood vessels and contribute to the development of atherosclerosis which heightens the risk of heart attacks, strokes, and peripheral artery disease. Additionally, diabetes often coincides with other risk factors like high blood pressure and abnormal cholesterol levels, compounding the cardiovascular risk. Conversely, individuals with CVD have a higher likelihood of developing diabetes due to shared risk factors and underlying mechanisms16. Thus, managing blood sugar levels through proper diabetes management, adopting a heart-healthy lifestyle, and closely monitoring cardiovascular health is crucial for those with diabetes to mitigate the increased risk of CVDs.
Nutrition and Lifestyle
Proper nutrition plays a pivotal role in mitigating the risk of CVD. A well-balanced diet rich in fruits, vegetables, whole grains, low fat sources of protein, and healthy fats can significantly contribute to heart health17. Consuming high-fibre foods aids in reducing cholesterol levels and maintaining healthy blood pressure18. Minimizing saturated fats, as well as excessive salt and added sugars, is key to preventing the development of conditions like atherosclerosis and hypertension17.
Omega-3 fatty acids, found in fatty fish, walnuts, and flaxseeds, are known to lower inflammation, improve cholesterol profile and blood function, and ultimately reduce cardiovascular risk17. Moreover, antioxidants from colourful fruits and vegetables combat oxidative stress, which is linked to CVD17. By making thoughtful dietary choices and incorporating heart-friendly nutrients, individuals can enhance their cardiovascular well-being and reduce the risk of heart-related complications, ultimately promoting a healthier, more resilient heart.


Lifestyle factors also have a profound impact on cardiovascular health. Regular physical activity is a cornerstone in reducing the risk of CVD. Engaging in aerobic exercises like brisk walking, jogging, or cycling enhances heart and improves blood circulation, and helps maintain a healthy weight19.
Avoiding tobacco products is paramount, as smoking significantly raises the risk of CVD20. Additionally, managing stress through techniques like meditation, yoga, or deep breathing might help control some risk factors associated with CVD21.
Limiting alcohol consumption and adhering to recommended guidelines is crucial for heart health, as excessive drinking can lead to high blood pressure and heart muscle damage. By adopting a physically active lifestyle, abstaining from smoking, managing stress, and moderating alcohol intake, individuals can proactively safeguard themselves against CVD and foster a heart-healthy life19.
Heart Health
Randox Health advocates for a proactive and preemptive approach to ensure optimal well-being and vitality. Our mission is to revolutionize the healthcare paradigm, shifting away from reactive disease management and embracing a proactive strategy for prevention. Through comprehensive assessments that encompass a range of vital indicators, including those related to heart health, Randox Health empowers individuals to assume control over their health trajectory.
By identifying potential risk factors at their earliest manifestations, we aim to equip individuals with the knowledge needed to make informed decisions rooted in scientific expertise. Our goal is to guide individuals toward strategies that enhance their long-term cardiovascular health and minimize the likelihood of heart disease and stroke.

To help you take a proactive approach to your heart health, Randox Health provide the Vital Health Check. Vital measures more than 20 key biomarkers related to your heart and diabetic health to provide you with an assessment of your risk of heart disease, stroke, and diabetes. Testing of your cardiac risk is also included within the Everyman/Everywoman packages and Signature programmes.
References
- Davis L. Body Physics: Motion to Metabolism. Vol 1. 1st ed. Open Oregon Educational Resources; 2020.
- British Heart Foundation. How are blood vessels made? Heart Matters Magazine . Published 2023. Accessed September 28, 2023. https://www.bhf.org.uk/informationsupport/heart-matters-magazine/research/how-are-blood-vessels-made
- World Health Organisation. Cardiovascular diseases (CVDs). https://www.who.int/health-topics/cardiovascular-diseases.
- John Hopkins Medicine. Atherosclerosis . https://www.hopkinsmedicine.org/health/conditions-and-diseases/atherosclerosis.
- Shahjehan RD, Bhutta BS. Coronary Artery Disease. StatPearls; 2023.
- Oijha N, Dhamoon AS. Myocardial Infarction. StatPearls Publishing ; 2023.
- Huff T, Boyd B, Jialal I. Physiology, Cholesterol.; 2023.
- Navar AM. The Evolving Story of Triglycerides and Coronary Heart Disease Risk. JAMA. 2019;321(4):347. doi:10.1001/jama.2018.20044
- Olofsson SO, Wiklund O, Borén J. Apolipoproteins A-I and B: biosynthesis, role in the development of atherosclerosis and targets for intervention against cardiovascular disease. Vasc Health Risk Manag. 2007;3(4):491-502.
- Kronenberg F, Mora S, Stroes ESG, et al. Lipoprotein(a) in atherosclerotic cardiovascular disease and aortic stenosis: a European Atherosclerosis Society consensus statement. Eur Heart J. 2022;43(39):3925-3946. doi:10.1093/eurheartj/ehac361
- Bays HE, Taub PR, Epstein E, et al. Ten things to know about ten cardiovascular disease risk factors. Am J Prev Cardiol. 2021;5:100149. doi:10.1016/j.ajpc.2021.100149
- John Hopkins Medicine. Types of Stroke . https://www.hopkinsmedicine.org/health/conditions-and-diseases/stroke/types-of-stroke.
- National Heart Lung and Blood Institute. Causes and Risk Factors. Stroke. Published May 26, 2023. Accessed September 28, 2023. https://www.nhlbi.nih.gov/health/stroke/causes
- Wang X, Dong Y, Qi X, Huang C, Hou L. Cholesterol Levels and Risk of Hemorrhagic Stroke. Stroke. 2013;44(7):1833-1839. doi:10.1161/STROKEAHA.113.001326
- World Heart Federation. ATRIAL FIBRILLATION. https://world-heart-federation.org/world-heart-day/cvd-causes-conditions/atrial-fibrillation/.
- Sharma A, Mittal S, Aggarwal R, Chauhan MK. Diabetes and cardiovascular disease: inter-relation of risk factors and treatment. Futur J Pharm Sci. 2020;6(1):130. doi:10.1186/s43094-020-00151-w
- Casas R, Castro-Barquero S, Estruch R, Sacanella E. Nutrition and Cardiovascular Health. Int J Mol Sci. 2018;19(12):3988. doi:10.3390/ijms19123988
- Reynolds AN, Akerman A, Kumar S, Diep Pham HT, Coffey S, Mann J. Dietary fibre in hypertension and cardiovascular disease management: systematic review and meta-analyses. BMC Med. 2022;20(1):139. doi:10.1186/s12916-022-02328-x
- Tian D, Meng J. Exercise for Prevention and Relief of Cardiovascular Disease: Prognoses, Mechanisms, and Approaches. Oxid Med Cell Longev. 2019;2019:1-11. doi:10.1155/2019/3756750
- Gallucci G, Tartarone A, Lerose R, Lalinga AV, Capobianco AM. Cardiovascular risk of smoking and benefits of smoking cessation. J Thorac Dis. 2020;12(7):3866-3876. doi:10.21037/jtd.2020.02.47
- Manchanda SC, Madan K. Yoga and meditation in cardiovascular disease. Clinical Research in Cardiology. 2014;103(9):675-680. doi:10.1007/s00392-014-0663-9



