06/11/2023
Prostate cancer, the most common form of cancer in men, can be a difficult topic and one many men would rather avoid, this article aims to clear up some of the myths about prostate cancer and help you to better understand the role of prostate cancer testing.
What is the Prostate?

The prostate is a small, walnut-sized gland located below the bladder. Its primary role is to produce the white fluid that, when mixed with sperm, creates semen2.
The prostate itself is divided into zones or anatomic regions. Prostate cancer most commonly forms in the peripheral region, the one at the back or closest to the rectum. In these cases, the doctor may request a digital rectal exam (DRE)3. This is an examination that involves the doctor inserting a gloved finger into the rectum to examine the prostate first-hand. This examination can’t be used alone as a definitive diagnosis; therefore, it will normally be accompanied by a PSA test3.
What is Prostate Cancer?
Prostate cancer is the most common form of cancer in men. In the UK, 1 out of 8 men will receive a prostate cancer diagnosis within their lifetime. It is estimated that 12,000 men die every year from prostate cancer… that’s 1 death every 45 minutes5.
Cancer typically arises when cells start multiplying rapidly, leading to the formation of a tumour. This abnormal growth often occurs due to the absence of a ‘stop’ signal that typically restrains cell proliferation when necessary6. Once established, certain cancers utilise androgens (sex hormones influencing male development) as a source of sustenance, fuelling further expansion. Some types of prostate cancer progress slowly and are often identified before spreading beyond the prostate. Yet, this delayed growth pattern poses a challenge as prostate cancer commonly exhibits no distinct symptoms, complicating its detection and potentially allowing it to metastasise (spread) beyond the prostate6.
Risk Factors
Prostate cancer is mostly diagnosed in men over 50 years old. Unlike some other cancers, it is not strongly associated with a wide range of modifiable risk factors, but there are a few factors that are known to increase risk:
Age
Getting older is a major risk factor for prostate cancer. It mainly affects men aged 50 or over. Men under 50 can get prostate cancer but it isn’t common.
If you have a family history of prostate cancer or breast cancer your risk is increased. It is estimated that 20% of prostate cancer patients report a family history of the disease7. You are two and a half times more likely to get prostate cancer if your father or brother has had it.
In the UK about 1 in 4 Black men will get prostate cancer in their lifetime.
Prostate Cancer Testing – PSA
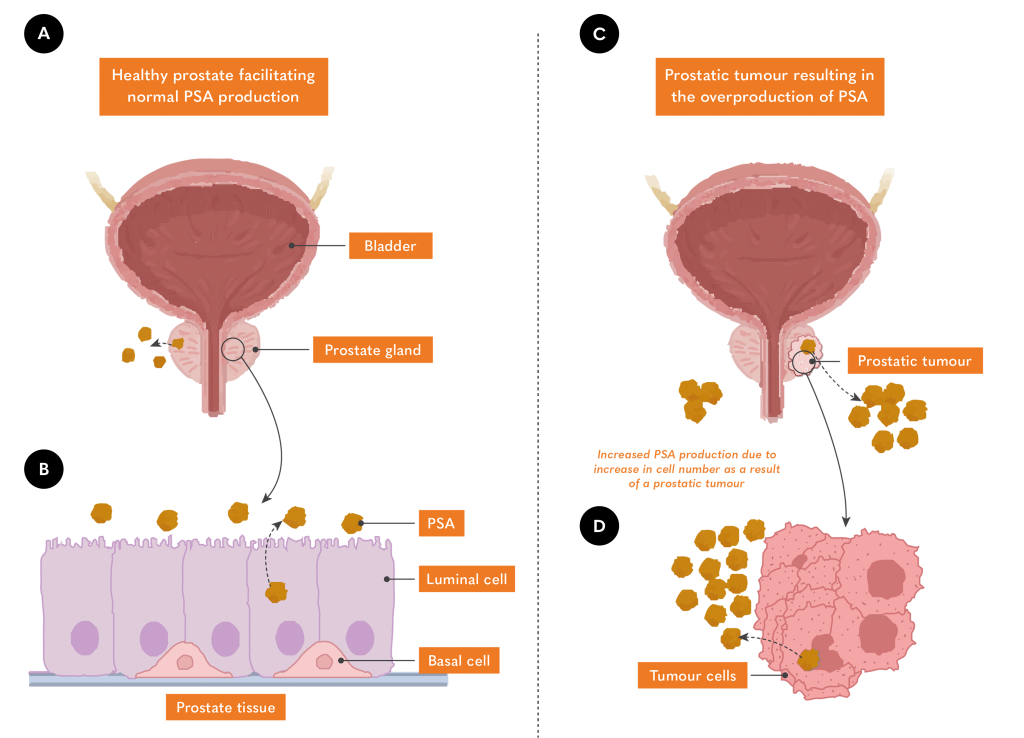
Normal PSA levels vary in the population and increase with age, however, men aged between 50-69 are expected to have a PSA level of <3 nanograms per ml8. PSA levels can be elevated due to several mechanisms:
- When prostate cancer eliminates certain cells, it can disrupt the structure of the prostate, allowing more PSA to enter the bloodstream.
- The increased number of cells caused by prostate cancer tumours express PSA in addition to that produced by healthy prostate cells, driving the increase in PSA concentration.
Prostate cancer testing using standard PSA can be tough as elevations are not specific to prostate cancer. High PSA levels might mean an enlarged prostate, prostatitis, or a urinary infection. Furthermore, research shows that 3 out of 4 men with high PSA won’t have prostate cancer8. However, PSA testing is a useful indicator and is used throughout the world to estimate risk and support diagnosis.
Myths about Prostate Cancer
In the age of misinformation, deciphering fact from fiction can be a hard nut to crack. Here, we will take a quick look at some of the myths swimming around in relation to prostate cancer.
"Getting a vasectomy causes prostate cancer"
This myth has been around for a while, there’s no strong evidence that this is the case. A meta-analysis showed that there was a link between vasectomy and prostate cancer. However, when only considering the most robust and high-quality analysis, this association becomes weaker and less significant. In other words, it may be the case that there is some link, but it is unlikely that vasectomy directly causes prostate cancer9.
Sexual activity increases the risk of developing prostate cancer
It was rumoured that lots of sexual activity or frequent ejaculation increased the risk of prostate cancer. Another myth! Scientists have found no evidence of this. In truth, researchers at Harvard discovered the exact opposite, a decreased risk for men with high ejaculation frequency10.
Genetic Testing at Randox Health
At Randox Health we believe in a proactive approach to your health. There are 3 main contributing factors to risk of prostate cancer: age, family history and ethnicity. This is why we have developed our Prostate Cancer Risk test. This test investigates the genome at 12 distinct sites, to identify potentially harmful variants in the genetic code. Having one of these genetic variants does not mean that a person will develop prostate cancer but does suggest that they are at increased risk. You can read about some of these genetic variants below:
Everyone has BRCA1 and BRCA 2 genes, their function is to keep your cells growing normally and prevent the growth of cancer cells. If you have a genetic variant in one of these genes it can change the gene and cause it not to work properly. Men with a BRCA2 gene variant are at a higher risk of developing prostate cancer. Your risk may only be slightly increased if you have a BRCA1 gene variant. Having a BRCA gene variant does not mean you will get prostate cancer but you are at higher risk.
This variant is associated with a higher-than-average risk of developing prostate cancer11,12, however, the variant accounts for a small fraction of all prostate cancers12.
The gene TP53 is responsible for producing the protein known as p53. This protein has earned the nickname ‘guardian of the genome’ because of its critical involvement in essential functions like regulating the cell cycle, initiating programmed cell death, managing metabolism, and repairing DNA. Men who have TP53 mutations are thought to be predisposed to a particularly aggressive form of prostate cancer13.
There’s a lot to consider before deciding to go ahead with genetic screening.
Genetic counselling is crucial for informed decision-making on genetic testing. These experts meticulously review the individual’s and their family’s medical history, pinpointing possible genetic concerns. This holistic approach determines the appropriateness of genetic testing.
After opting for genetic testing, counsellors provide invaluable assistance in interpreting the results. They elucidate the implications for the individual’s health and their family members and discuss strategies for managing any emerging issues. This could involve recommending closer monitoring or preventive measures.
With all genetic screening at Randox Health, you can book an appointment with a genetic counsellor who will help empower you with the knowledge to navigate genetic risks and make informed choices for your well-being. If you or someone you know would like to find out about risk of prostate cancer, information on how to book an appointment is available here: https://randoxhealth.com/en-GB/in-clinic/prostate-cancer-risk and don’t forget to book a consultation with one of our Genetic Counsellors.
Prostate Cancer Testing at Randox Health
At Randox Health, we also offer advanced Prostate Health testing for those who wish to investigate their risk of prostate disease. As we’ve mentioned, PSA isn’t specific to prostate cancer; it may indicate prostatitis, an enlarged prostate, or a urinary tract infection. This is why, in addition to PSA, our advanced PSA test includes analysis of a novel combination of biomarkers to generate a prostate cancer risk score, which can significantly improve the predictive potential of PSA alone in identifying individuals at risk of prostate cancer.
- Samant R, Balchin K, Cisa-Paré E, et al. The importance of humour in oncology: a survey of patients undergoing radiotherapy. Curr Oncol. 2020;27(4):e350-e353. doi:10.3747/co.27.5875
- NHS. Prostate Cancer. Health A to Z. Published October 18, 2021. Accessed October 23, 2023. https://www.nhs.uk/conditions/prostate-cancer/
- Prostate Cancer Foundation. Prostate Gland. What is Prostate Cancer. Published 2023. Accessed October 23, 2023. https://www.pcf.org/about-prostate-cancer/what-is-prostate-cancer/prostate-gland/
- Harvard Health. PSA: Prostate-Specific Antigen, Persisting Scientific Ambiguities. Harvard Health Blog. Published July 1, 2009. Accessed October 23, 2023. https://www.health.harvard.edu/newsletter_article/PSA-Prostate-Specific-Antigen-Persisting-Scientific-Ambiguities
- Prostate Cancer Foundation. About prostate cancer. Prostate Cancer UK. Published 2023. Accessed October 23, 2023. https://prostatecanceruk.org/prostate-information-and-support/risk-and-symptoms/about-prostate-cancer
- Prostate Cancer Foundation. How Prostate Cancer Grows. What is Prostate Cancer. Published 2023. Accessed October 23, 2023. https://www.pcf.org/about-prostate-cancer/what-is-prostate-cancer/how-it-grows/
- Rawla P. Epidemiology of Prostate Cancer. World J Oncol. 2019;10(2):63-89. doi:10.14740/wjon1191
- NHS Choices. Should I get a PSA test? NHS. Published 2019. Accessed October 23, 2023. https://www.nhs.uk/conditions/prostate-cancer/should-i-have-psa-test/
- Baboudjian M, Rajwa P, Barret E, et al. Vasectomy and Risk of Prostate Cancer: A Systematic Review and Meta-analysis. Eur Urol Open Sci. 2022;41:35-44. doi:10.1016/j.euros.2022.04.012
- Havard Health. Ejaculation frequency and prostate cancer. Men’s Health.
- Nyberg T, Tischkowitz M, Antoniou AC. BRCA1 and BRCA2 pathogenic variants and prostate cancer risk: systematic review and meta-analysis. Br J Cancer. 2022;126(7):1067-1081. doi:10.1038/s41416-021-01675-5
- Ewing CM, Ray AM, Lange EM, et al. Germline mutations in HOXB13 and prostate-cancer risk. N Engl J Med. 2012;366(2):141-149. doi:10.1056/NEJMoa1110000
- Maxwell KN, Cheng HH, Powers J, et al. Inherited TP53 Variants and Risk of Prostate Cancer. Eur Urol. 2022;81(3):243-250. doi:10.1016/j.eururo.2021.10.036
- Mental Health Foundation. Men and mental health. Explore Mental Health. Published October 1, 2021. Accessed October 24, 2023. https://www.mentalhealth.org.uk/explore-mental-health/a-z-topics/men-and-mental-health



