04/08/2023
As part of our Signature and Digestive Health Packages, we include a bowel/gut health test to helping to identify potential issues relating to gastrointestinal health. Employing our ground-breaking algorithms, these tests can help detect several gastrointestinal conditions. In this article, we will investigate these conditions, the factors which increase your risk of developing these conditions, and the preventative action you can take in order to improve your health.
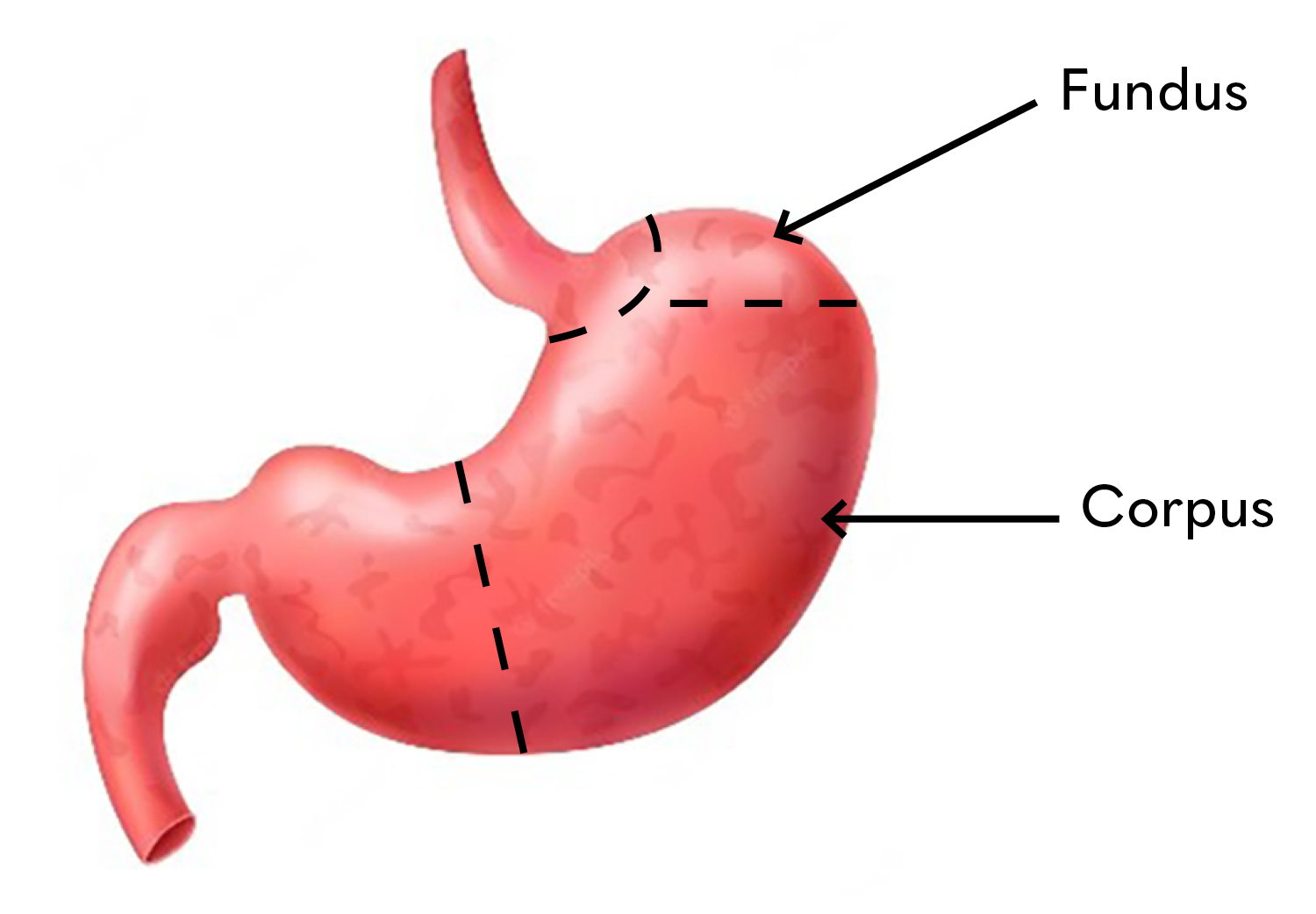
Autoimmune Atrophic Gastritis
Autoimmune atrophic gastritis is common in Western countries, affecting up to 5% of the population4. It is a chronic autoimmune disease caused when the body’s immune system attacks the parietal cells in the gut, which are responsible for producing stomach acid and intrinsic factor (IF)1. IF is necessary for the absorption of vitamin B12, which is essential to produce healthy red blood cells. Without sufficient levels of IF, one can develop pernicious anaemia, a condition characterized by vitamin B12 deficiency and a lack of healthy red blood cells3. As well as increasing the risk of vitamin B12 malabsorption, autoimmune atrophic gastritis has been associated with an increased risk of gastric cancer.
Autoimmune atrophic gastritis mainly affects the main body of the stomach, known as the corpus and the upper portion of the stomach, known as the fundus. It may not cause any symptoms, particularly in the early stages of the disease before the development of vitamin B12 deficiency. When they do occur, symptoms of autoimmune atrophic gastritis can include:
- upper abdominal pain or discomfort
- nausea
Then as vitamin B12 deficiency develops, further symptoms may include:
- fatigue
- weakness
- shortness of breath
- dizziness
- pale skin
- tingling or numbness in fingers or toes
- irritability
- low mood
Sound Familiar?
Our standalone digestive-bowel health screening provides a hollistic overview of your gut health with the intention of:
- Indicating gut health.
- Analyse the risk of gastritis, stomach ulcers and stomach cancer.
- Distinguish between Inflammatory Bowel Disease (IBD) & Irritable Bowel Syndrome (IBS).
Helicobacter pylori Gastritis
Helicobacter pylori (H. pylori) gastritis is a common bacterial infection of the stomach lining that can cause chronic inflammation, stomach ulcers, and in rare cases, stomach cancer. H. pylori bacteria are thought to be transmitted through contaminated food, water, or close contact with an infected person. Once in the stomach, the bacteria attach to the lining and produce toxins that damage the cells and cause inflammation.
The prevalence of H. pylori infection varies widely depending on geographic location and socioeconomic factors, but it is estimated that up to 50% of the global population is infected with the bacteria4.
H.Pylori Breath Testing
In addition, untreated H.pylori infection is a known cause of stomach cancer, with infection causing 41% of stomach cancer cases in the UK (Stomach cancer risk | Cancer Research UK).
Prevention of these conditions always will trump treatment. Get ahead of the curve by testing early, identifying risks and ultimately protecting your future health.
In developed countries, the prevalence is lower, but still significant, with around 30-40% of the population affected1. Most people infected with H. pylori will not experience any symptoms. However, those that do are likely to experience abdominal pain, bloating, nausea, vomiting, and in some cases, loss of appetite, weight loss, and fatigue5.
Treatment typically involves a combination of antibiotics and acid-reducing medications to eradicate the bacteria and promote the healing of the stomach lining. An early gut health test/diagnosis and treatment are paramount to prevent complications and promote healing of the stomach lining
Gastric Cancer
Stomach or gastric cancer is a type of cancer that develops in the cells that line the stomach. It is the fifth most common cancer worldwide and the third leading cause of cancer-related deaths, with an estimated 1 million cases and 768,000 deaths in 20206 However, figures are lower in the UK with around 6500 new cases per year it is the 17th most common cancer7.
Several risk factors have been identified for stomach cancer, including age, gender, diet, and environmental factors such as exposure to certain chemicals. In addition, untreated H.pylori infection is a known cause of stomach cancer, with infection causing 41% of stomach cancer cases in the UK7. Men are at a higher risk of developing stomach cancer than women, and the risk increases with age. People who have a family history of stomach cancer, especially a first-degree relative, are at an increased risk of developing the disease8. Additionally, a diet high in salt, smoked or processed meats, and low in fruits and vegetables is associated with an increased risk of stomach cancer9.
Preventing stomach cancer involves eradication of H. pylori in those infected and reducing exposure to risk factors such as a high salt diet, smoking, and environmental exposure to things such as asbestos, coal dust or chemicals like benzene. A diet high in fruits, vegetables, and fibre has been associated with a reduced risk of stomach cancer10. A Regular stomach cancer or gut health test is also recommended for people at high risk, including those with a family history of the disease11.
Hyperchlorhydria and Hypochlorhydria
Hyperchlorhydria and hypochlorhydria are conditions related to the amount of acid in the stomach. Both conditions can cause discomfort and affect digestion, but they differ in the level of acidity present. Hyperchlorhydria is the condition where the stomach produces too much acid, while hypochlorhydria is the opposite; the stomach doesn’t produce enough acid. Both conditions can result in similar symptoms, such as abdominal pain, heartburn, and bloating.
The symptoms of hyperchlorhydria and hypochlorhydria can be similar, but they differ in severity. Hyperchlorhydria can cause heartburn, indigestion, nausea, and vomiting12. In contrast, hypochlorhydria can lead to nutrient deficiencies, fatigue, bloating, and abdominal discomfort13.
Several risk factors can contribute to the development of hyperchlorhydria and hypochlorhydria. Environmental factors, such as stress, smoking, and alcohol consumption, can increase the risk of hyperchlorhydria14. Meanwhile, hypochlorhydria can be caused by chronic inflammation of the stomach lining, autoimmune disorders, or the use of certain medications. Genetic factors may also play a role in the development of these conditions15.
Treatments for hyperchlorhydria include medications such as proton pump inhibitors and H2 blockers may be prescribed to reduce the production of stomach acid16. Lifestyle changes, such as reducing stress, avoiding trigger foods, and quitting smoking, can help manage symptoms. Hypochlorhydria can be treated by replacing the deficient stomach acid with supplements, and in some cases, antibiotics may be needed to treat bacterial overgrowth17.
Coeliac Disease
Coeliac disease is a chronic autoimmune disorder that damages the small intestine of genetically predisposed individuals when they consume gluten, a protein found in wheat, barley, and rye. The condition affects approximately 1 in 100 people globally, with a prevalence that varies across regions and ethnic groups18.
The exact cause of Coeliac disease is unknown, but the condition is believed to be a combination of genetic, environmental, and immunologic factors. Individuals with a family history of the condition are at higher risk of developing it, as are those with autoimmune disorders such as type 1 diabetes, rheumatoid arthritis, and autoimmune thyroid disease19.
Coeliac disease can present with a range of symptoms that can vary in severity and onset. Common symptoms include abdominal pain, bloating, diarrhoea, constipation, and nausea. Other symptoms can include fatigue, bone or joint pain, weight loss, and skin rashes20. Left untreated, coeliac disease can lead to several serious complications, including malnutrition, osteoporosis, infertility, and an increased risk of certain cancers such as lymphoma and small bowel cancer21.
In-Clinic Genetic Coeliac Testing
Through a DNA test at ANY of our health clinics, measure risk of coeliac disease developing in you or your close family members.
The only effective treatment for coeliac disease is a lifelong gluten-free diet. This involves avoiding all foods that contain gluten, including bread, pasta, and beer. Individuals with coeliac disease need to be vigilant when reading food labels and when eating out, as even small amounts of gluten can cause damage to the small intestine22.
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) is a group of chronic gastrointestinal disorders that cause inflammation in the digestive tract. Ulcerative colitis (UC) and Crohn’s disease (CD) are the most common forms of IBD, and they affect millions of people worldwide. Although these conditions share some similarities, they also have distinct characteristics and require different treatments.
Ulcerative colitis (UC) is a chronic inflammatory disorder that affects the large intestine (colon) and rectum. The exact cause of UC is unknown, but it is thought to be an autoimmune condition in which the immune system attacks healthy tissue in the colon, leading to inflammation and ulcers. Risk factors for UC include a family history of the disease, age (most often diagnosed in people between the ages of 15 and 35), and ethnicity23.
Symptoms of UC can range from mild to severe and include diarrhoea (often with blood or pus), abdominal pain and cramping, rectal pain, fatigue, and unintended weight loss. If left untreated, UC can lead to serious complications such as colon cancer, perforated colon, severe bleeding, and toxic megacolon24.
Crohn’s disease (CD) is another type of chronic inflammatory bowel disease that can affect any part of the digestive tract, from the mouth to the anus, unlike UC, which only affects the colon and rectum. The exact cause of CD is also unknown, but it is believed to be an autoimmune disorder that occurs when the immune system attacks healthy tissue in the digestive tract25.
Risk factors for CD include a family history of the disease, age (most often diagnosed in people between the ages of 15 and 35), and smoking25.
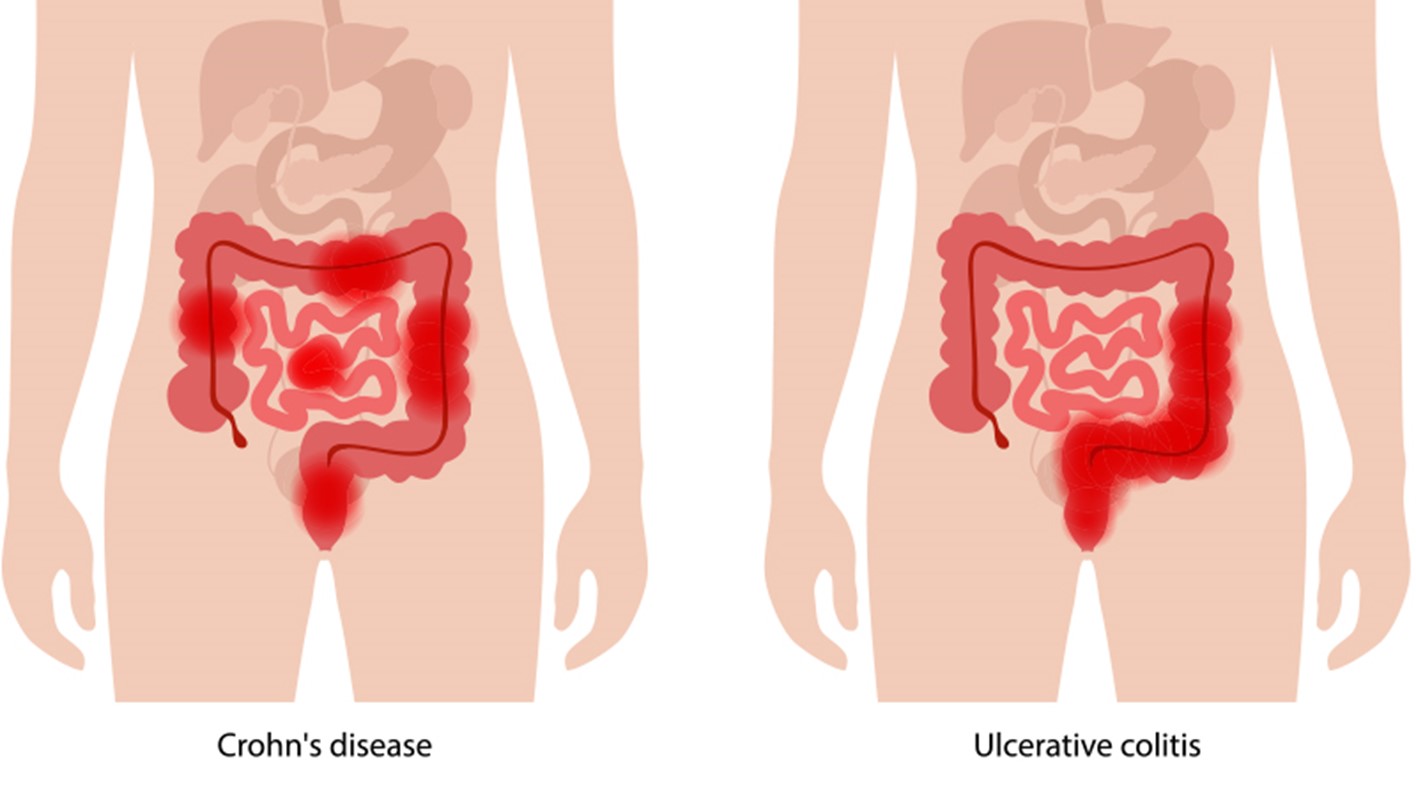
Symptoms of CD can vary depending on the location and severity of inflammation and can include diarrhoea, abdominal pain and cramping, fatigue, unintended weight loss, and a reduced appetite. In severe cases, CD can cause complications such as bowel obstruction, fistulas, abscesses, and malnutrition26.
Although there is no cure for IBD, both UC and CD can be managed with the help of medication, lifestyle changes, and in some cases, surgery27.
A Gut Health Test at Randox Health
At Randox Health, our state-of-the-art gut health tests can identify potential biomarkers associated with a wide range of gastrointestinal disorders. Using this data and our innovative algorithms we can provide you with valuable information relating to your risk of developing the gastrointestinal conditions discussed in this article. With this information, you can make informed decisions about your health and take appropriate actions to prevent or manage any potential health issues.
If you’re worried about the risk of any of the conditions investigated within, seek support from Randox Health. Our team of healthcare professionals can assist you with testing and interpretation of your results, as well as provide guidance on how to manage the condition and prevent complications. By acting with our help, you can proactively improve your digestive health and minimize potential health risks.
Reference List
- Chey, W. D., & Leontiadis, G. I. (2017). Howden, CW. ACG clinical guideline: treatment of Helicobacter pylori infection. American Journal of Gastroenterology, 112(2), 212-239
- Lahner, E., & Annibale, B. (2012). Pernicious anemia: new insights from a gastroenterological point of view. World Journal of Gastroenterology, 18(21), 2773-2780. doi: 10.3748/wjg.v18.i21.2773
- Wang, X., Li, W., & Zhang, D. (2019). Association between autoimmune gastritis and pernicious anemia. Advances in Clinical and Experimental Medicine, 28(8), 1101-1105. doi: 10.17219/acem/104152
- Bago, J., Dominguez-Munoz, J. E., & Sostres, C. (2016). Helicobacter pylori infection and gastric acid secretion. Gastroenterology and Hepatology from Bed to Bench, 9(2), 70–77.
- Graham, D. Y., & Fischbach, L. (2010). Helicobacter pylori treatment in the era of increasing antibiotic resistance. Gut, 59(8), 1143-1153.
- Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 71(3), 209-249.
- Cancer Research UK. Stomach cancer statistics. Cancer Research UK. Published May 14, 2015. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/stomach-cancer#heading-One
- S. National Library of Medicine. (2021). Stomach Cancer. MedlinePlus. Retrieved from https://medlineplus.gov/stomachcancer.html
- Kato, I., & Tahara, E. (2014). Review of the epidemiology of stomach cancer. Asian Pacific Journal of Cancer Prevention, 15(22), 9811-9815.
- World Cancer Research Fund / American Institute for Cancer Research. (2018). Diet, Nutrition, Physical Activity and Stomach Cancer. Continuous Update Project Expert Report.
- S. National Library of Medicine. (2021). Stomach Cancer Prevention. MedlinePlus.
- Vakil N, van Zanten SV. Kahrilas PJ, Dent J, Lauritsen K, Malfertheiner P, et al. Gastro-oesophageal reflux disease. Lancet. 2013;381:1933-1942.
- Kornbluth A, Sachar DB, Practice Parameters Committee of the American College of Gastroenterology. Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010;105(3):501-523.
- Ness-Jensen E, Hveem K, El-Serag H, Lagergren J. Lifestyle interventions in the management of gastroesophageal reflux disease: a systematic review. World J Gastroenterol. 2016;22(27):6250-6265.
- Palsson-McDermott EM, O’Neill LA. The Warburg effect then and now: from cancer to inflammatory diseases. Bioessays. 2015;37(10):999-1007.
- Fass R, Ofman JJ. Gastroesophageal reflux disease—should we adopt a new conceptual framework? Am J Gastroenterol. 2013;108(5):705-709.
- Lacy BE, Chey WD, Lembo AJ. New and emerging therapies for functional dyspepsia. Gastroenterology. 2017;152(5):924-938.
- Lebwohl B, Sanders DS, Green PHR. Coeliac disease. Lancet. 2018;391(10115):70-81.
- Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA. ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol. 2013;108(5):656-76.
- Catassi C, Kryszak D, Louis-Jacques O, et al. Detection of celiac disease in primary care: a multicenter case-finding study in North America. Am J Gastroenterol. 2007;102(7):1454-60.
- Ludvigsson JF, Leffler DA, Bai JC, et al. The Oslo definitions for coeliac disease and related terms. Gut. 2013;62(1):43-52.
- Vakil, N., van Zanten, S. V., Kahrilas, P. J., Dent, J., & Lauritsen, K., et al. (2013). Gastro-oesophageal reflux disease. The Lancet, 381(9881), 1933-1942. doi: 10.1016/S0140-6736(13)60607-6
- Baumgart DC, Sandborn WJ. Inflammatory bowel disease: clinical aspects and established and evolving therapies. The Lancet. 2007;369(9573):1641-1657.
- Loftus EV. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology. 2004;126(6):1504-1517.
- Cosnes J. Tobacco and IBD: relevance in the understanding of disease mechanisms and clinical practice. Best Practice & Research Clinical Gastroenterology. 2004;18(3):481-496.
- Feuerstein JD, Cheifetz AS. Crohn’s disease: epidemiology, diagnosis, and management. Mayo Clinic Proceedings. 2017;92(7):1088-1103.
- Kornbluth A, Sachar DB; Practice Parameters Committee of the American College of Gastroenterology. Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. American Journal of Gastroenterology. 2010;105(3):501-523



