08/01/2024
More and more people, every year, are deciding to participate in Dry January. The idea is simple: No alcohol for the whole month of January. Drinking is deeply embedded in world culture and people have many reasons to drink. From celebrations and parties to the fear of missing out. From the quiet pint during the week, to the heavy weekend sessions. Those who drink are all too aware of the side effects of alcohol. The stress relief, the confidence boost; the anxiety, the fear. You probably also know that long term, or excessive short-term drinking can have some serious effects on your body, most commonly your liver.
Therefore, rather than associating Dry January with depriving yourself of something, perhaps it’s an opportunity to develop some new, healthy habits. Here are some things to consider that might help if you’re thinking about taking a break from drinking:
This old adage is a cliché for a reason. One of the most common reasons for drinking is to relieve stress. But is this really the case? While it can seem like a good release, and a reason to socialise, the stress relief is only ever temporary. Whether it’s the fear of what you did last night, going to work on Monday groggy and tired or checking your bank account after a heavy weekend, most of our trips to the pub result in more stress, not less. Instead, try other ways to relieve stress such as exercise, getting out into nature, yoga, or all the above!
Rather than thinking about all the things you’re missing by not drinking, like the headache, the dry mouth, and the exhaustion, perhaps consider all the things you stand to gain.
- No hangovers
- Better sleep
- Less anxiety
- Improved mental clarity
- Brighter eyes and skin
- More money in the bank
A positive attitude can make all the difference when it comes to changing your mindset. By enduring Dry January rather than enjoying it, you’re going into the year giving up your head start.
The idea that “life is short, so enjoy it” is usually positive. However, when this belief leads to behaviours like excessive drinking, it creates a paradox. On one hand, we’re told to cherish life, and on the other, we engage in activities that may cut it short. Seems counterproductive. Balancing enjoyment of the present with choices that support long-term well-being is key in resolving this contradiction.
The misuse of alcohol is responsible for over 3 million deaths globally every year1, many of which are caused by alcoholic liver disease (ALD). Years or decades of drinking can damage almost all your organs, but in most cases, it is the liver that takes the initial and most of the damage.
Alcohols are a class of chemical compounds. The one we find in our beverages is ethanol. Ethanol is metabolised in the liver, primarily by the liver’s parenchymal cells which make up 70% of the livers mass2. These cells produce a variety of enzymes which break down ethanol. The byproducts of this chemical breakdown increase fat, or lipid, accumulation in the liver; reduce the breakdown of these fats; and increase oxidative stress and inflammation in the liver2. These features are what causes ALD. Liver disease can be categorised into 4 stages: Steatosis, Steatohepatitis, Fibrosis and Cirrhosis.
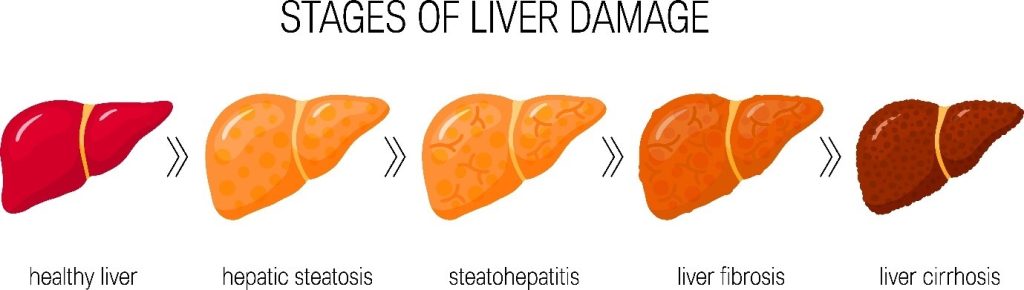
Steatosis means fatty liver, or more accurately the accumulation of fat in the liver. This stage is often asymptomatic and can develop after decades of moderate drinking or after binge drinking, defined as 4-5 regular drinks within 2 hours2. The good news is this stage is commonly reversible with positive lifestyle changes and reducing your alcohol intake3. Steatohepatitis describes stage 2. At this stage, the accumulation of fat has caused inflammation of the liver, the result of which, is liver cell death2. Once enough liver cells have died, we reach stage 3 – Fibrosis. The dead liver cells produce collagen which accumulates into fibres, or scar tissue. Scarring of the liver is the first sign of irreversible damage2.
The final stage is known as cirrhosis, named after the Greek, kirrhos (yellowish) + osis (state or condition). Cirrhosis describes severe fibrosis that affects the livers’ ability to carry out its essential functions; metabolism, detoxification, and protein synthesis to name a few2.
The stages of ALD are similar to that of Non-Alcoholic Fatty Liver Disease (NAFLD), otherwise known as Metabolic-dysfunction Associated Steatotic Liver Disease (MASLD). Up to 30% of people around the world are thought to suffer from one of the above stages of liver disease4.
What makes NAFLD different from ALD is exactly what you think, its not related to alcohol, or in the MASLD definition, it is the result of metabolic dysfunction4. Like ALD, non-alcoholic liver disease can take years to progress, so it’s important to know your risk of liver disease, whether you’re a big drinker or not.
Bringing It Back To Dry Jan.
We hope we’ve said enough to convince to take a break from drinking for the month of January and perhaps beyond. If you’re going to give it a go, here’s a few tips which might help succeed or help motivate you further.
Recruit a friend – You can hold each other accountable and encourage each other, especially if you are the competitive type.
Tell people! – This will not only help with holding yourself accountable, but will give others a heads up that you might not be in the pub for a while
Keep a diary – Keeping a record of the month can help you track the positive changes you notice over the month. Who knows? You might even look back and decide a life of sobriety is for you after all.
Have Fun – Plan some fun activities for the month. Do something new. Take that class. Try that walking trail you managed to avoid all last year. The important thing is that you experience the positives of not being in the pub or hungover.
Mocktails! – If you still want to or must attend functions or places with alcohol, try non-alcoholic alternatives. Its common for places have extensive ranges of non-alcoholic cocktails and drinks which in many cases, taste little different than the alcoholic ‘real thing’.
If you’re interested in discovering more about your liver health, consider our Liver Health Test (https://randoxhealth.com/en-GB/in-clinic/liver-health) . This package includes biomarkers related to kidney function as well as a FibroScan®, a non-invasive method of analysis levels of liver scarring.
- World Health Organisation. Alcohol. Fact Sheets. Published May 9, 2022. Accessed December 13, 2023. https://www.who.int/news-room/fact-sheets/detail/alcohol
- Osna NA, Donohue TM, Kharbanda KK. Alcoholic Liver Disease: Pathogenesis and Current Management. Alcohol Res. 2017;38(2):147-161.
- British Liver Trust. NAFLD, NASH and fatty liver disease. https://britishlivertrust.org.uk/information-and-support/liver-conditions/non-alcohol-related-fatty-liver-disease/.
- Chan WK, Chuah KH, Rajaram RB, Lim LL, Ratnasingam J, Vethakkan SR. Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): A State-of-the-Art Review. J Obes Metab Syndr. 2023;32(3):197-213. doi:10.7570/jomes23052



